Adoptive Cell Therapy in Cancer Treatment
Updated on Feb 5, 2025 Share
Adoptive Immunotherapy
The human body is naturally equipped with tools to fight off infectious diseases and harmful pathogens. An intricate system of cells works together to facilitate an immune response that defends the body from dangerous substances. Although this process is both fast and adaptive, there are limitations to what it can do. Certain diseases, such as cancer, can intensify to a point where the immune system is no longer capable of fighting the disease on its own. Adoptive cell therapy, or cellular immunotherapy, is a method that uses and manipulates T cells to find innovative ways of treating cancer.
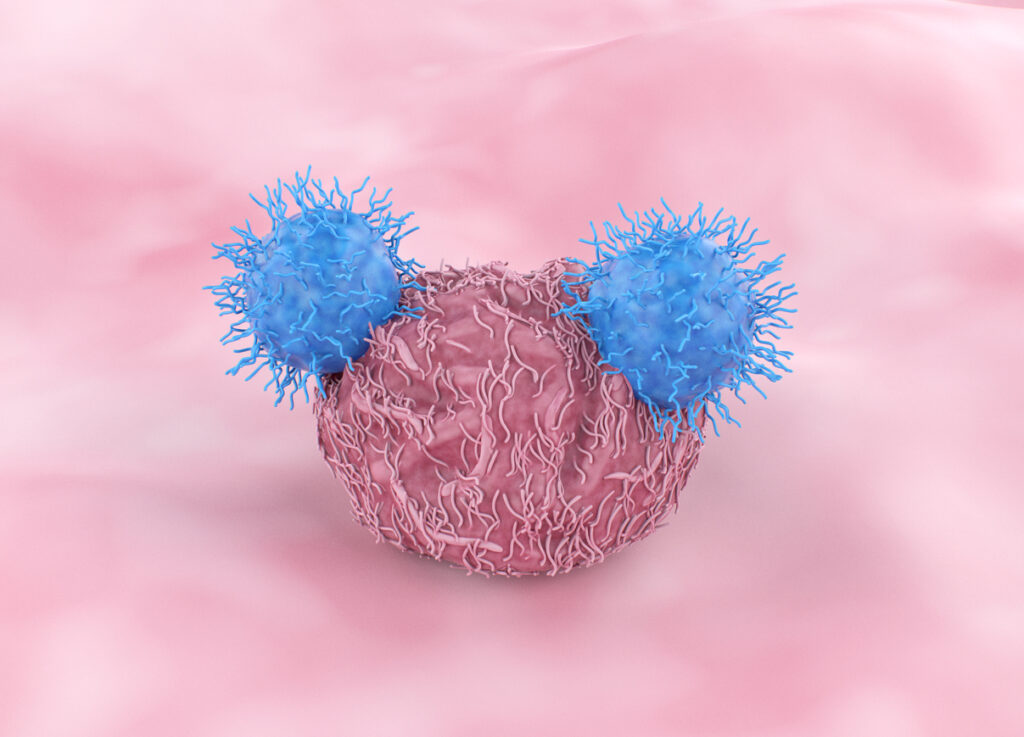
These strategies include multiplying T cells to keep up with an influx of developing cancer cells or using gene therapy to alter and enhance our cells’ abilities to fight tumors. Cytotoxic (CD8+) T cells are known for their ability to fight cancerous cells by identifying their surface marker antigens and eliminating them. Adoptive cell therapy harnesses this technique through multiple processes such as:
- Tumor-infiltrating lymphocyte (TIL) therapy
- Engineered T cell receptor (TCR) therapy
- Chimeric antigen receptor (CAR) T cell therapy
- Natural killer (NK) therapy
Each one of these strategies has its own limitations and works best on specific populations. They all continue to be updated with new medical advances to make them as effective as possible.
Immunotherapy Methods
Cell immunotherapies are in a constant state of change because they are still relatively new in the medical field. Many are still under scrutiny for their long-term effects and how they interact in combination with other treatments. Accessibility to isolated T cells is essential for medical research to continue in these areas.
Tumor-Infiltrating Lymphocyte Therapy
When a patient develops a cancerous tumor in their body, the immune system recognizes it as a threat and attempts to resolve the problem. T cells are released that can recognize the surface antigens of the tumor and cells related to it. Cancer is rapid and unregulated cell reproduction — even though cytotoxic T cells can effectively kill tumor cells, the rate at which new cancer cells are produced can overwhelm the body’s defenses.
On top of needing a large number of T cell to fight a tumor, these lymphocytes must be activated if they are to successfully destroy the harmful cells. The amount of T cells that are both activated and set to target the cancer antigens is too low to maintain an adequate response against cancer for extended periods of time.
Perhaps the simplest immunotherapy treatment method involves isolating T cells that have already been activated to fight cancer cells and multiplying them outside of the body. After increasing the amount of cancer-specific cytotoxic T cells, the sample is reintroduced into the bloodstream through an IV. This method is called tumor-infiltrating lymphocyte therapy and can aid the body’s natural immune response without.
Engineered T Cell Receptor Therapy
Some patients don’t develop activated cells that have recognized their tumor. Since there are no specialized cells to replicate, existing cells must be altered to carry out the desired function. In engineered T cell receptor therapy, new TCRs are attached to T cells that allow them to bind to the cancer cells present in the body. This also allows doctors to more accurately target different types of tumors; creating a more personalized treatment plan for patients and hopefully creating a better outcome in the long run.
CAR T Cell Therapy
TIL and TCR therapy both rely on the surface antigens of cancer cells having recognizable major histocompatibility complex (MHC) molecules. The MHC is responsible for marking cells and creating a docking station to signal cytotoxic T cells. Without the MHC the body would not be able to respond to any foreign pathogens as the T cells would not be able to recognize them as a threat.
Advancements in the field of immunotherapy have led to the development of chimeric antigen receptor T cell therapy. This process involves equipping a synthetic receptor to T cells that’s capable of binding to naturally occurring antigens on the surface of tumor cells. This renders previously untouchable cancer cells vulnerable to the modified cytotoxic T cells.
CAR T cell therapy differs from TCR therapy in the type of receptors that are placed onto the cells. In TCR, T cells are engineered to bind to the MHC markers the immune system attaches to tumor cells. CAR on the other hand, uses a synthetic receptor that attaches to natural receptors on the tumor cells. Together these methods allow doctors to treat a wider variety of cancers the body is not capable of handling on its own.
Natural Killer Therapy
Another immunotherapy treatment that doesn’t rely on MHC molecules is natural killer therapy. Natural killer therapy is when another type of lymphocyte called a killer cell is supplemented with CAR receptors. Killer cells normally roam the bloodstream eliminating harmful cells in a similar fashion to cytotoxic cells, but they attack pathogens without MHC receptors.
NK therapy takes lymphocytes that wouldn’t normally attack tumorous cells and equips them with receptors for naturally occurring antigens. This strategy expands the ways in which doctors can treat different cancers. In a situation where one strategy isn’t successful, it’s always beneficial to have an alternative.
T Cell Isolation
One thing the immunotherapy methods all have in common is the need for T cell isolation. TIL, TCR, CAR, and NK therapy all require lymphocytes to be separated and oftentimes purified. The importance of T cells in the field of immunology means there’s a lot to consider when choosing a cell separation technique.
Not only is it significant to factor in the costs of the chosen strategy, the time required for each process should also be taken into account. Some of the more traditional methods call for complex and specific devices that take a lot of effort to learn and store. Fluorescence activated cell sorting and magnetic-activated cell sorting are also known for their cell loss. These sortation techniques lose cells from hydrodynamic stress and a harsh magnetic field respectively.
Microbubble Technology
The alternative to these methods is called buoyancy activated cell sorting (BACS). BACS uses small bubbles to draw the target cells away from other substances in the sample. By linking the microbubbles with antibodies that will also link with marked antigens on the surface of the targeted population, the cells will be gently dragged to the top of the solution.
After this separation occurs the cells on the top can be easily collected for closer observation or removed so the leftover cells at the bottom may be studied. BACS works faster than the other methods of cell separation for only a fraction of the cost. Small kits are added to a sample and stirred for 5-15 minutes — the bubbles do the rest. The bubbles are tough enough to hold their form but soft enough not to harm their passengers as they travel around the sample.
Check Out Akadeum’s Products
Akadeum’s microbubble technology isolates T cells quickly and effectively at a relatively low cost when compared to other traditional methods. For simple T cell separation and RBC depletion try our products today.


