CAR T Cells: How These Cancer Fighting T Cells are Harvested and Manufactured for Immunotherapy
Updated on Dec 10, 2024 Share
Immunotherapy
Immunology is the study of the immune system and what it can do, immunotherapy is the study of how to do things the immune system can’t do. In immunotherapy, researchers observe and manipulate T cells in the body in an effort to make up for humans’ natural deficiencies. There are multiple methods of immunotherapy — each for different purposes. While some strategies merely extract T cells for a population increase then reintroduce them to the bloodstream, others go so far as to engineer and attach new antigens.
Chimeric Antigen Receptor T Cells
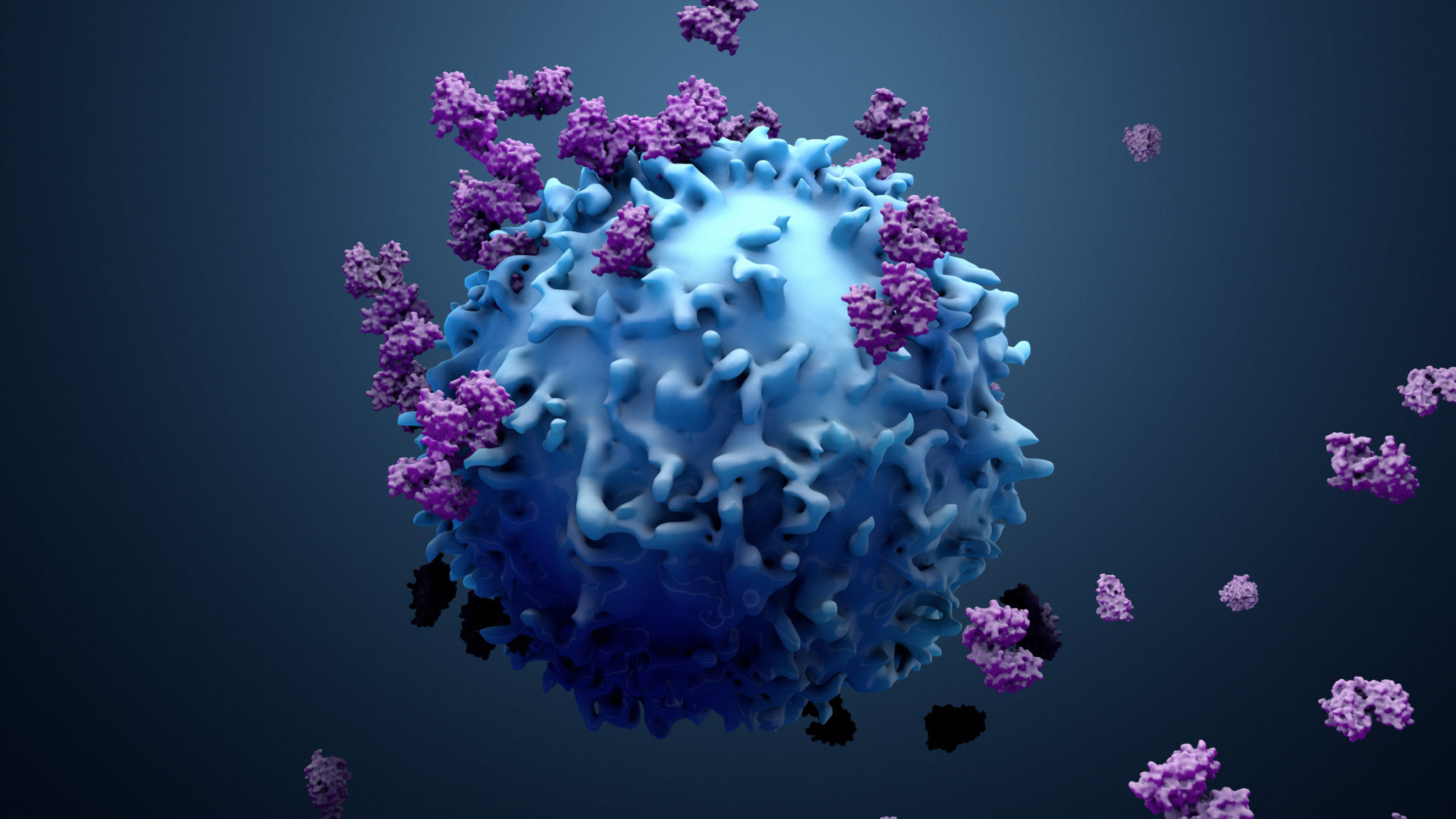
One method of immunotherapy for cancer treatment is the use of chimeric antigen receptor (CAR) T cells. Like foreign cells in the body, immune system T cells have receptors on their surface. These two proteins act like a lock and key, with a receptor being able to recognize a corresponding antigen. CAR T cell research aims to find new ways to treat cancer by capitalizing on this unique trait.
CAR T cells have been modified with a receptor that allows them to bind to the naturally occurring antigens on cancer cells. These T cells normally only recognize cells that have MHC molecules attached to them. This means they can only combat certain types of cancer cells that the body is able to decipher and place a mark on.
Cancer Treatment
When a tumor is present in the body it sheds fragments into the bloodstream called circulating tumor cells (CTCs). These cells float around and have the potential to create more tumors throughout the body. Depending on the surface antigen specific to the variation of cancer, cytotoxic (CD8+) T cells may not be able to eliminate the harmful cells. CAR T cells can be programmed to attack the variations that the body doesn’t naturally recognize.
For example, certain cases of lymphoma and leukemia will have cancer cells that display an antigen called CD19 on the surface. CD19 is not recognized by MHC receptors, meaning the body won’t see these cells as a threat and therefore won’t attack them. With CAR T cells, the lymphocytes can be programmed to target the CD19 receptor. This technology allows the treatment of cancers that were previously untouchable. CAR T cells made to bind to these antigens will not be able to bind to any others.
FDA Approved Treatments
The Food and Drug Administration (FDA) regulates the research and sale of products that pertain to human health in the United States of America. Innovative cancer treatments and potentially dangerous medical procedures fall under the FDA’s jurisdiction. Due to the risk that exists with such a young technique, only a small handful of heavily tested treatments are currently approved.
The first approved therapy is called brexucabtagene autoleucel, or Tecartus. This strategy is only viable for patients with mantle cell lymphoma that haven’t responded to other treatments. Mantle cell lymphoma targets B cells in the body and spreads very quickly. Though there are still harmful side effects in some patients, the FDA has ruled Tecartus as a last effort treatment because there’s a higher chance of remission for those who continue to relapse.
Axicabtagene ciloleucel, also called Yescarta, is the second therapy supported by the FDA. Yescarta can treat patients with a few different types of B-cell lymphoma, further expanding upon Tecartus. To be eligible for this treatment patients must undergo an extensive evaluation and have already attempted systemic therapies.
The last approved method is tisagenlecleucel, or Kymriah. While it can also treat a form of lymphoma, this CAR T cell therapy is additionally capable of treating adults with acute lymphoblastic leukemia. This form of leukemia happens to have the same CD19 receptors as lymphoma which allows the CAR T cells to recognize and attack it. Like Yescarta and Tecartus, Kymriah only becomes an approved treatment method after other strategies have failed and the patient is running out of options.
CD19 is the first antigen a CAR T cell has been developed for, but further research is underway for a variety of others. There’s currently active research and clinical trials for treatment of carcinoma (PSMA), glioblastoma (GD2), and breast cancer (HER2). Between research and practical uses, the demand for isolated T cells is greater than ever.
Manufacturing CAR T Cells
Prior to the widespread application of these techniques, scientists must have a reliable source of high-quality CAR T cell products; this is only possible through the process of manufacturing. The clinical CAR T cell manufacturing process is a critical step that involves isolating, purifying, and engineering T cells.
Before cells can be manufactured, they must be collected from a T cell source. In most cases, the source collection occurs from the peripheral blood mononuclear cells of the patient. Physicians will choose a window of time when the number of T lymphocytes is high to ensure sufficient presence in the sample. This allows the researcher to build a crop of T cells for further activation and modification.
Once T cells are collected, isolated, and purified with cell separation, they must be activated to fight cancer cells. An inactivated T cell will not have the tools to fight harmful substances it binds to in the body. The activation can occur with natural hormones from the body or be artificially triggered from an antigen presenting cell.
The final step of manufacturing is the modification of receptors. Until the T cells are modified, they do not become CAR T cells. Chimeric antigen receptors are attached to the surface of the cell with viral or non-viral gene transfer systems. The receptor is expressed on the activated cell and they merge to create a cancer cell assassin.
Limitations
The manufacturing process comes with a vast array of limitations that make it difficult to keep up with the rising demands. CAR T cell manufacturing platforms are currently labor intensive — they take a lot of time and work. The one-to-one nature of CAR T cells to specific cancer types makes it difficult to produce the cells in bulk. Multiple samples need to be engineered in parallel to proportionally increase the amount of research that can be done across the entire field. The amount of work required to run each of these complex tasks consequently causes the necessary goods to be very expensive. Without an abundance of resources, the potential for CAR T cell research is low.
However, there are ways to make the manufacturing process quicker and cheaper that should be considered whenever possible. Perhaps the area where the most resources can be saved is during cell separation. Depending on what technique is used to isolate the T cells from blood samples, large amounts of time and money can be saved. That’s why Akadeum developed a scalable and high throughput human T cell enrichment method.
Microbubbles
When it comes to T cell separation, the most cost and time effective method is buoyancy activated cell separation, or BACS. This process harnesses tiny bubbles to lift target cells to the top of a solution. By using the same antigen-receptor combo as previously explained, the microbubbles are bound to a substance. After linking together, the buoyant properties gently lift the target to the top to be collected or removed. The whole process takes 5-15 minutes and is less expensive than other traditional methods.
Check Out Akadeum Today
BACS can help to lighten the cost of CAR T cell manufacturing along with a multitude of other research endeavors. If you’re looking for a simple and effective way to isolate T cells, look no further than Akadeum’s microbubble products.