TIL Therapy: Revolutionizing Solid Tumor Treatment
Updated on Nov 20, 2024 Share
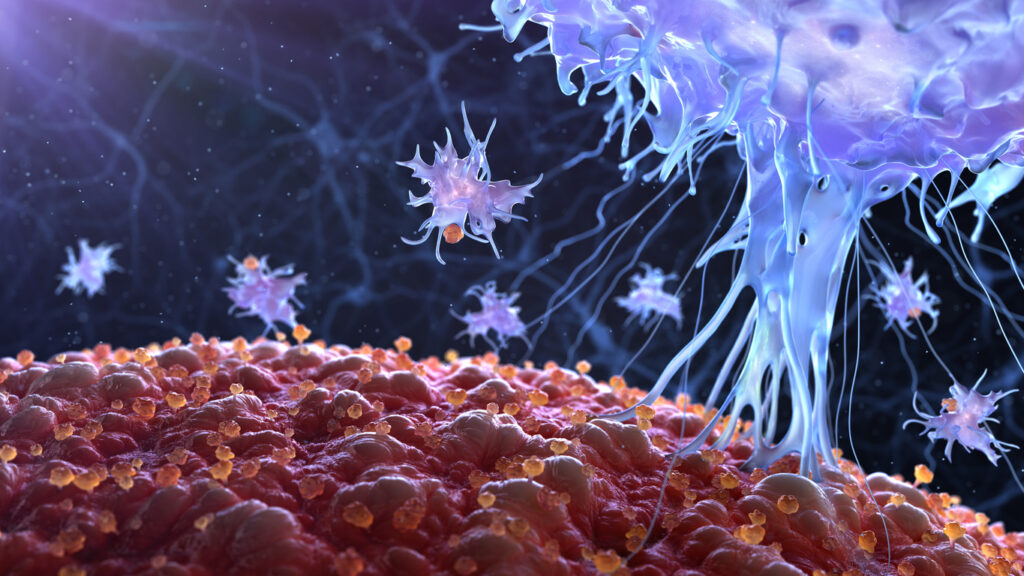
Tumor-infiltrating lymphocyte (TIL) therapy is a modern cancer treatment used to combat notoriously hard-to-treat solid tumors. Like other adoptive cell therapies, TIL harnesses the body’s immune system to combat malignancies by using T cells, a type of white blood cell integral to immune response. Except in TIL therapy, these T cells are directly extracted from tumors.
Having survived the tumor microenvironment, these lymphocytes are already primed to recognize and attack cancer cells, offering a personalized approach to cancer immunotherapy. Unlike traditional treatments that often have a broader target, TIL therapy is specifically tailored to each patient’s unique tumor, increasing the potential for effective treatment outcomes. This innovative method reflects a significant shift in oncology, emphasizing the role of individualized treatment strategies in combating various forms of cancer.
TIL Therapy Process
Tumor-infiltrating lymphocyte therapy is a multi-step process that mobilizes the body’s immune system to fight cancer. These are the major steps in creating an intricately tailored treatment for each patient:
- Extraction of TILs: The process begins by surgically removing a piece of the patient’s tumor, from which TILs are extracted. These lymphocytes are already fighting the cancer but are typically outnumbered within the tumor environment.
- Expansion and activation: Once isolated, these TILs are taken to a laboratory where they are cultured and stimulated to proliferate. This step involves the use of cytokines, such as interleukin-2 (IL-2), to activate and expand the TILs, significantly increasing their numbers and enhancing their ability to fight tumor cells.
- Reinfusion into patients: After sufficient expansion, these activated TILs are infused back into the patient. Prior to the reinfusion, patients typically undergo a lymphodepletion regimen, including chemotherapy, to reduce the number of other immune cells in the body. This step enhances the effectiveness of the infused TILs.
- Post-infusion monitoring: Following the reinfusion, the patient’s response to the cell therapy is closely monitored. The expanded TILs, now in large numbers, navigate through the body to locate and destroy cancer cells.
- Supportive care: Patients often receive additional treatments, such as IL-2-based immunotherapy medications, to support the TILs’ activity.
This therapy has shown promise in treating various types of cancers, particularly those where other treatments have failed. Its effectiveness lies in the personalized approach, using the patient’s immune cells to target the tumor. However, the process is complex and requires facilities and expertise found only at specialized cancer centers.
Clinical Trials of TIL Therapy in Cancer
TIL therapy has been explored and applied in various types of tumor cells with varying degrees of success. It has shown significant efficacy in treating metastatic melanoma, where it’s often effective even in cases resistant to other treatments.
For example, one of the largest studies of patients with anti-PD-1-refractory advanced melanoma treated with TIL therapy shows promising results. A trial by Targeted Therapies in Oncology, focusing on the use of lifileucel, demonstrated durable efficacy with an objective response rate (ORR) of 31.4%. The treatment’s safety profile aligns with known profiles of lymphodepletion and IL-2, with a decreasing incidence of treatment-emergent adverse events over time. A Food and Drug Administration (FDA) decision on this treatment’s approval is expected in the first half of 2024.
Research and trials are also underway to assess its effectiveness in treating cervical and ovarian cancers, with some cautiously promising early results. The application of TIL therapy in other solid tumors, such as those in gastrointestinal, breast, and lung cancer, is being actively investigated. Each cancer type presents its unique challenges and responses to TIL therapy, making continued research essential for understanding and improving its effectiveness across different malignancies.
Challenges and Limitations of TIL Therapy
TIL therapy, while promising, faces significant challenges and limitations. T cell exhaustion, where infused T cells lose effectiveness over time, is a major concern. The therapy also requires specialized, labor-intensive procedures, limiting accessibility.
Additionally, patients treated with TIL often respond differently, impacting effectiveness. The therapy’s aggressiveness can sometimes lead to severe immune-related side effects, especially when combined with the side effects of the companion chemotherapy and IL-2 treatments.
Manufacturing and delivering TILs pose further logistical challenges, and personalized treatment protocols for each patient complicate the process. These issues underscore the need for ongoing research to enhance TIL therapy’s efficacy and available treatment options.
Role of Cell Separation in TIL Therapy
Cell separation occurs after the tumor tissue containing TIL cells is removed from the patient. Separating the effective immune cells from the tumor without damaging them is vital to the success of TIL therapy. Traditional cell separation methods, such as centrifugation and filtration, often fall short of maintaining cell integrity.
Centrifugation, for instance, relies on spinning cells at high speeds to separate them based on density. While effective in separating cell types, this method can be hard on cells, potentially leading to damage and reduced viability. Filtration methods, which involve passing cell mixtures through physical barriers, can also be detrimental due to the mechanical stress they impose on cells.
The various types of flow cytometry are known for high specificity, sorting cells based on multiple parameters, and providing detailed cell analysis. However, these techniques require expensive equipment and expertise, can be time-consuming, and may cause cell damage as TILs are herded through the system’s microfluidics.
Alternatively, magnetic-activated cell sorting (MACS) is relatively quick and cost-effective. However, MACS has lower specificity compared to flow cytometry and requires specialized equipment.
Akadeum’s Microbubble Technology Enhances TIL Therapy
In contrast to traditional techniques, new modern techniques like Akadeum’s microbubble technology have proven to be a significant advancement in cell separation. This innovative method employs tiny, biodegradable microbubbles coated with specific functionalized molecules like streptavidin or antibodies. These molecules are designed to bind selectively to target cells. When introduced into a mixture of cells, the microbubbles attach to the cells and gently float them to the surface, separating them from other cell types with minimal stress.
This buoyancy-activated cell sorting (BACS™) technique offers several advantages:
- It is less invasive and damaging to the cells compared to traditional methods, ensuring higher cell viability.
- It provides a higher degree of purity in the separated cells, which is crucial for the effectiveness of TIL therapy.
- The process is efficient and can be scaled up, making it suitable for clinical applications where a large number of cells are required.
The advancement of cell separation techniques, particularly the introduction of gentle and efficient methods like Akadeum’s microbubble technology, plays a pivotal role in enhancing the efficacy of TIL therapy. By ensuring the integrity and purity of TILs, these modern techniques contribute significantly to the success of this innovative cancer treatment approach.
To learn how Akadeum’s microbubble technology can benefit your therapy research, contact our team of experts today.


