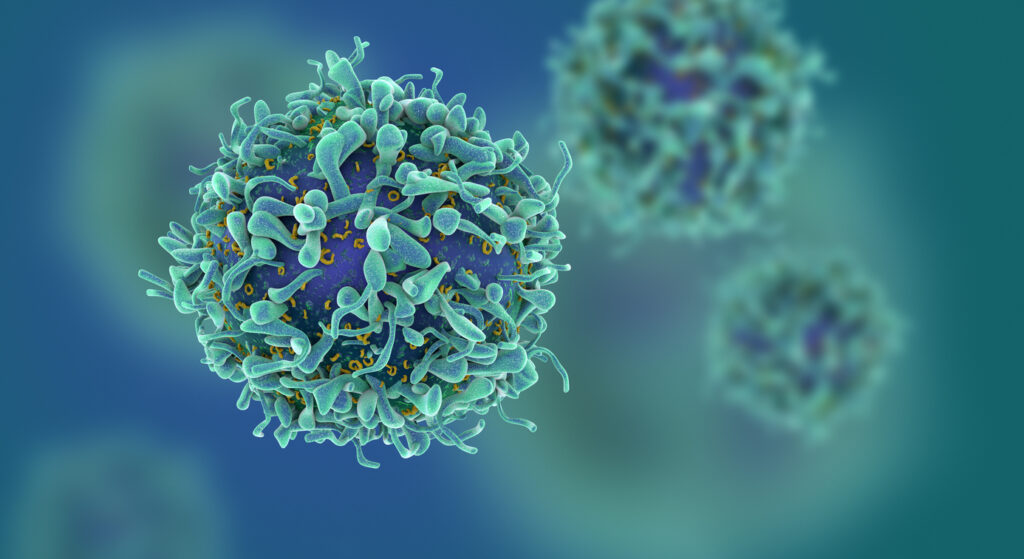
T-Cell
T cells, also known as T lymphocytes, are white blood cells that mature in the thymus, a specialized immune system organ. They help protect the body from infections and cancer. There are several types of T cells, each specialized to carry out specific immune functions in response to pathogens or viruses. For example, helper T cells (CD4+) assist other white blood cells, while cytotoxic T cells (CD8+) directly attack infected cells.
T cells are part of adaptive immunity, which provides targeted and specific defenses against foreign invaders like bacteria, allergens, and hazardous endogenous cells like cancer cells. Read on to discover more about T cells’ maturation process and functions in the immune system.
How Do T Cells Function in the Immune System?
T cells are responsible for recognizing potential threats by responding to antigens and initiating a targeted inflammatory response. Antigens are small molecules or fragments of molecules that elicit a response from the immune system. The unique receptor found on the surface of T cells, called the T cell receptor (TCR), binds to antigens present in the body and triggers the T cell to be activated, initiating an immune response. The TCR is highly specific and will only trigger T cell activation upon exposure to its unique antigen.
Once activated, T cells undergo clonal expansion. This process produces a large number of identical T cells with the same TCR specificity. The significant expansion and amplification of specialized T cells after exposure to its antigen is the hallmark of proper T cell activation and function.
There is also a mass release of cytokines from T cells during activation that signals to other immune cells that a threat has been identified. T cells can directly destroy infected or suspicious cells or recruit help from other immune cells to amplify the attack. After the threat has been defeated, regulatory T cells diminish the inflammatory response, triggering apoptosis in T cells that are no longer needed. Some T cells remain as memory T cells to ensure a quick and efficient response in the case of re-exposure. This is called “immunologic memory.”
The Life of a T Cell
T cell precursors originate in the bone marrow from stem cells. They traffic to the thymus for T cell development and maturation and are equipped with surface markers that allow them to interact with antigens and determine self and non-self antigens. These cells are vetted thoroughly through multiple rounds of selection within the thymus to eliminate T cells unable to distinguish self-antigens from foreign ones as well as T cells that react too strongly to self-antigens.
After maturing T cells migrate throughout the bloodstream and tissues, circulating through secondary lymphoid organs and the lymphatic system where they will most likely encounter their specific antigen. During this stage, they are considered “naive” T cells. At this time in the T-cell lifespan, they do not possess effector functions, like cytokine release or cytotoxic abilities. Once activated, these cells quickly navigate to wherever they are needed to fight the current pathogen, continuously scanning for their specific antigen.
During an immune response, T cells can be found in the peripheral tissues, such as the site of an infection. T cells are the front lines of the immune response, with some T cell subsets directly killing infected cells.
Types of T Cells
There are different types of T cells, each serving a unique immune function. These functions are determined by a combination of developmental checkpoints as well as education in the periphery after exposure to an antigen.
1. Helper T Cells
Helper T cells, or CD4+ T cells, coordinate the immune response. They communicate the threat to other immune cells—like B cells—through the release of signaling, such as cytokines. These act on other cells, including immune cells and non-immune cells, inducing them to aid in the immune response. CD4 is a protein surface marker unique to helper T cells, which functions as a coreceptor for the TCR.
2. Cytotoxic T Cells
Also known as killer T cells, cytotoxic T cells can directly destroy pathogens or infected cells. By recognizing antigens on the surface of these abnormal cells, cytotoxic T cells’ effector abilities are activated, leading to the release of perforin and granzymes, which kill the infected cell. Cytotoxic T cells are identified by the surface marker CD8 and are also called CD8+ T lymphocytes.
3. Regulatory T Cells
The intense inflammation caused by T cell activation, when left unregulated, can cause significant damage to the body. T regulatory cells (Tregs) are critical to maintaining immune system homeostasis and limiting overactive immune responses. They can suppress an excessive immune response by releasing signaling molecules that limit the effector function of other immune cells. Tregs are essential to protecting the body from the harmful effects of prolonged inflammation.
4. Memory T Cells
Very few T cells remain after an infection has been eliminated; most undergo apoptosis when they are no longer necessary. Memory T cells continue to circulate throughout the body to be ready to respond in the event of re-exposure.
Memory T cells allow the immune system to seemingly “remember” having encountered it before and respond rapidly and robustly upon re-exposure. Their ability to recognize specific antigens and quickly orchestrate targeted responses makes T cells a vital tool against disease.
T Cell Markers
T cell surface markers are proteins present on the surface of T cells by which they can be identified. These markers play integral roles in the development of the T cell, as well as its activation and eventual function. CD3 is the most common T cell marker and is associated with the TCR. This makes CD3 unique to T cells. This protein facilitates signal transduction during the binding of TCR to its specific antigen.
CD4 and CD8 are associated with helper T cells and cytotoxic T cells respectively. They function as co-receptors with the TCR and help tailor the T cell’s effector response. CD28 and CD69 are important activation-related T-cell markers. CD25 (or IL-2 receptor alpha) is commonly found on Treg and activated effector T cells and interacts with cytokine IL-2 to regulate the inflammatory response.
T Cell Activation and the Importance of Antigens
Antigens and antigen recognition drive the activation of the immune system, but they are not the only requirement for the robust expansion that follows T cell activation. Antigens must be presented to T cells via antigen-MHC complex, formed by the binding of the antigen to a major histocompatibility complex molecule on the surface of an antigen-presenting cell (APC), such as a dendritic cell. The class of MHC molecule determines whether it can be bound by a helper T cell or cytotoxic T cell.
After the antigen that fits the unique TCR on the naive T cell surface is presented by an antigen-MHC complex, co-stimulatory signals are required to further amplify the immune response. Molecules like CD28 and its ligands interact to provide the necessary co-stimulation. Successful activation triggers a cascade of signaling events within the T cell, causing it to proliferate and differentiate.
T Cells and Diseases
There are several diseases caused by dysfunction, overactivation, or misregulation of T cells within the body. T-cell-related conditions can have genetic causes or can arise from infections, autoimmune responses, or immunodeficiencies. Some viruses, like human immunodeficiency virus (HIV) which progressively depletes helper T cells, directly target T cells. This makes the body sensitive to infections and cancers, typically leading eventually to acquired immunodeficiency syndrome (AIDS).
Autoimmune diseases result when the body’s T cells cannot properly differentiate between pathogen or foreign antigens and self-antigens, causing unnecessary inflammation and a hyperactive T cell state that can be deadly. Because the T cells of an individual with an autoimmune disorder cannot differentiate self from non-self antigens, the body launches inflammatory attacks on healthy tissue and cells. Certain autoimmune disorders like multiple sclerosis and type 1 diabetes cause life-altering symptoms and can require constant monitoring to ensure patient safety.
The development of some cancers is also linked to T cell dysfunction. When T cells grow and proliferate uncontrollably and cannot be regulated, T cell lymphomas occur. Diseases linked to T cells are complex and diverse, normally involving many other immune cells in addition to T lymphocytes. Understanding how T cells prevent infection and fight diseases is essential to understanding T cell-linked diseases and disorders.
T Cell Isolation: Unlocking Insights for Research and Therapy
Isolating pure populations of T cells and T cell subsets has become a groundbreaking step forward in both immune research and therapeutic settings. T cell isolation is a laboratory method to extract T cells from a mixed population of immune cells, such as whole blood or a leukopak. Isolating T cells allows researchers and clinicians to study T cells at a deep level to gain an understanding of their function, life cycle, behavior, and antigen response.
T cell isolation has been critical for gene expression and signal transduction studies, providing insight into how T cells function in immune responses and during immune surveillance. Isolated T cells are also valuable tools for vaccine development. T cells can be used to assess risks and responses to a vaccine candidate before administration to the patient.
An incredible breakthrough in T cell science has been the invention and development of adoptive T cell therapy. T cells are isolated directly from a patient and then expanded and improved within a laboratory. These activated and expanded cells are transfused back to the patient, providing them with the power to destroy cancer cells and combat infections.
T cells are also commonly used to monitor changes during the progression of a disease or treatment. A patient’s T cell count can indicate multiple health factors and is a crucial tool for assessing immune system status.
T Cell Isolation With Microbubbles
Access to pure populations of T cells is integral to numerous applications in both clinical and research settings. At Akadeum, we provide gentle cell sorting technology for T cell isolation for every application.
Isolate pure and untouched T cell subtypes using our unique antigen cocktails paired with our powerful microbubbles. Our line of T-cell products includes kits specified to isolate bulk T cells, CD4+ helper T cells, and naive T cells from multiple sample types. Access high-quality T cell populations with a quick and easy workflow that saves time and resources.
By targeting surface proteins not found on T cells, our microbubbles simply bind to and float unwanted cells to the surface of the sample, leaving the T cells themselves untouched. Contact our team to find the right kit for your project today and experience the difference between microbubble technology and other cell separation methods firsthand!