An In-Depth View of Allogeneic Cell Therapy
Adoptive cell therapies, such as CAR T-cell therapy and TIL, tumor-infiltrating lymphocyte therapy, were breakthroughs in cancer T-cell treatment and provided an option for many patients who otherwise would have been without one. By taking over natural mechanisms in the human immune system, cell therapies redirect inflammation against a tumor.
What Does Allogeneic Mean?
Cell therapy originated by harvesting a patient’s cells, modifying them in some way that improved their ability to target and/or kill cancer cells, and returning them to the patient via infusion. As an autologous cell therapy, this method was groundbreaking in biopharmaceuticals, but it had many pitfalls in large-scale practice. Researchers created allogeneic cell therapy to address some of these pitfalls and make cell therapy more accessible.
Allogeneic cell therapy harvests starting cell material from healthy donors rather than patients for expansion and clinical treatment. By using donors, the risk for immune rejection is higher than autologous cell therapy, but allogeneic treatment has the potential to be more accessible and affordable.
Typically, severely ill patients will not have sufficient cell supply to undergo leukapheresis successfully. The quantity of cells needed for cell therapy is significant, and cancer patients tend to have low cell counts and/or widely skewed populations of immune cells. Many cancer treatments, such as chemotherapies and radiation therapies can impair the function of immune cells, including T cells. This can cause downstream cell therapy end-product quality issues. In these cases, physicians may prefer to treat using allogeneic cell therapy.
The high cell count required for proper dosage incurs a constant demand for healthy cells. The allogeneic cell therapy manufacturing system can meet such significant demand due to donor cells being activated and expanded in stock lots, quality controlled, cryopreserved, and distributed upon necessity.
How Are T Cell Expansion of Cells Extracted From a Healthy Donor?
The qualifications of donors for allogeneic cell therapies are distinct. A vast donor pool is crucial for the scalability of therapy-bound starting cells to ensure commercial cell suppliers or treatment centers have reliable source starting cells. Donors undergo leukapheresis—white blood cells (WBC) are harvested from a donor’s peripheral blood using an apheresis machine which returns the WBC-depleted blood to the donor.
Steps of an Allogeneic CAR-T Workflow
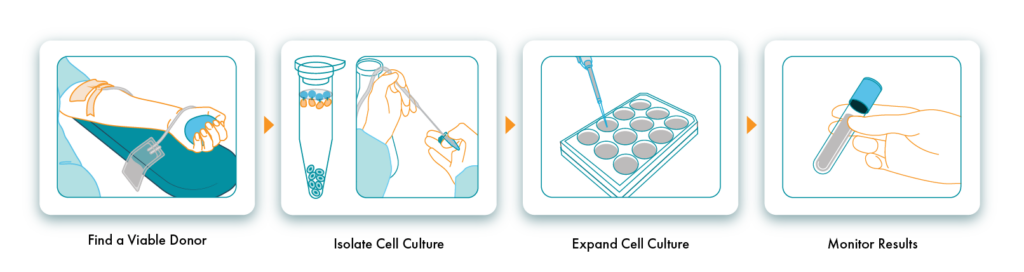
Find a Viable Donor
Studies have underscored the importance of human leukocyte antigen (HLA) matching of cell donors. HLAs are surface proteins on immune cells that regulate the immune response and help the immune recognition system differentiate between foreign and self-cells. A functioning immune system will launch an inflammatory response to foreign particles and cells that do not match the HLA profile.
Some donors have an exceptionally high HLA-matching rate and provide excellent starting material. However, these donors are hard to find and cannot be relied upon for continued donations. Treatment centers partnering with a cell supplier that sources from a curated donor pool make allogeneic cell therapy more available to patients.
Isolate and Expand Cell Culture
Once the donor has successfully undergone leukapheresis, the T cells are selected and are now ready for expansion. Many cell therapy manufacturers utilize large vessels that allow them to control media content and other cell culture conditions, called bioreactors, for the activation and expansion steps of allogeneic T-cell therapy.
These bioreactors perform T cell selection, activation, and expansion while maintaining an optimal cell culture environment. Expansion is the most critical step during the cell therapy manufacturing process and can take place at a much higher volume during allogeneic therapy than autologous therapy.
Monitor Results
In addition to the significant stock preparation abilities provided by allogeneic cell therapy manufacturing, quality control of allogeneic cells is also easier to monitor.
Limitations of Allogeneic CAR-T Therapy
Providing cell therapy at a lower cost and greater accessibility are the primary appeals of allogeneic cell therapy. However, there are still risks when using a donor supply of cells over a patient’s own cells.
Patient Rejection
When the infused cells recognize the healthy body cells as invading pathogens, the therapy cells may turn against the body, destroying patient cells. This phenomenon is called graft-versus-host disease, or GvHD. The resulting immune response is an undesired attack on the patient’s cells. GvHD is more likely in cases without a proper HLA match, highlighting the importance of adequate donor compatibility.
Allogeneic vs. Autologous Cell Therapy
Autologous cell therapy paved the way for allogeneic cell therapy, and both methods are still improving with ongoing research. Allogeneic cell therapy resolves many scaling issues plaguing autologous therapy, such as cost, accessibility, and supply/demand balance.
With autologous therapies, treatments are manufactured as needed. Alternately, allogeneic therapies can be prepared ahead and stored frozen until needed, greatly shortening the time-to-treatment for patients. The ease of logistics with shipping, freezing, and storing allogeneic therapy cells makes it ideal for wide-scale commercial clinical use.
Akadeum’s Cell Expansion and Isolation Methods
High-quality starting cellular materials are imperative to successful downstream activation and expansion. Allow Akadeum’s microbubble technology for cell therapy manufacturing to simplify isolation and selection steps. Our microbubble technology uses negative selection to produce untouched and unharmed cells ready for activation and expansion. Learn more about Akadeum’s T cell isolation kits and how to utilize them during a T cell culture and expansion protocol.


